Autoimmune diseases are when your immune system—your body’s germ-fighting equipment—gets turned around and attacks your own healthy cells. Imagine your body calling in the wrong type of backup and hurting you by mistake. This turning around can make you sick, cause ongoing inflammation, and hurt things like joints, skin, or organs.

These disorders are even more common than you might think. A massive 2023 Lancet study concluded that nearly one in every ten individuals on the planet has at least one autoimmune disorder. That’s a lousy lot of individuals! Some aren’t so bad, some are worse. If you treat them early and get good treatment, it really pays off.
Common Types of Autoimmune Diseases
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is when your body’s defense system attacks the lining of the joints. You might wake up stiff, sore, and swollen. If left alone, joints will become crooked. RA might even attack eyes, lungs, and other organs. But with good medications, most individuals live normal lives with RA.
Systemic Lupus Erythematosus
Physicians just call this one “lupus.” That way, the immune system can attack many parts of your body—skin, kidneys, heart, even the brain. People will get tired, have fevers, and sometimes get a butterfly-shaped rash on the face. Lupus is unpredictable and comes and goes erratically. Treatment is control of symptoms and calming the immune system.
Type 1 Diabetes
Type 1 diabetes occurs when your immune system attacks cells in your pancreas—these cells produce insulin, which your body uses to convert sugar to energy. It typically happens in childhood or early young adulthood. Type 1 diabetes individuals do not produce enough insulin, so they take injections or a pump for life. Most work very well with proper treatment, but they have to monitor their blood sugar closely.
Multiple Sclerosis
MS is when your immune system attempts to destroy the protective sheath of the nerve fibers of your brain and spinal cord. This disrupts messages in your nervous system and can cause numbness, weakness in your muscles, trouble with walking, or vision problems. MS can come back or even get worse over many years. Even though there is no cure yet, medication can slow it and ease symptoms.
Hashimoto’s Thyroiditis
This one strikes your thyroid gland in your neck and slows it down. The result? You may be weak, cold, depressed, gain weight, or simply tired all the time. Doctors treat Hashimoto’s with a small hormone tablet that replaces what your thyroid is no longer producing.
Causes of Autoimmune Diseases
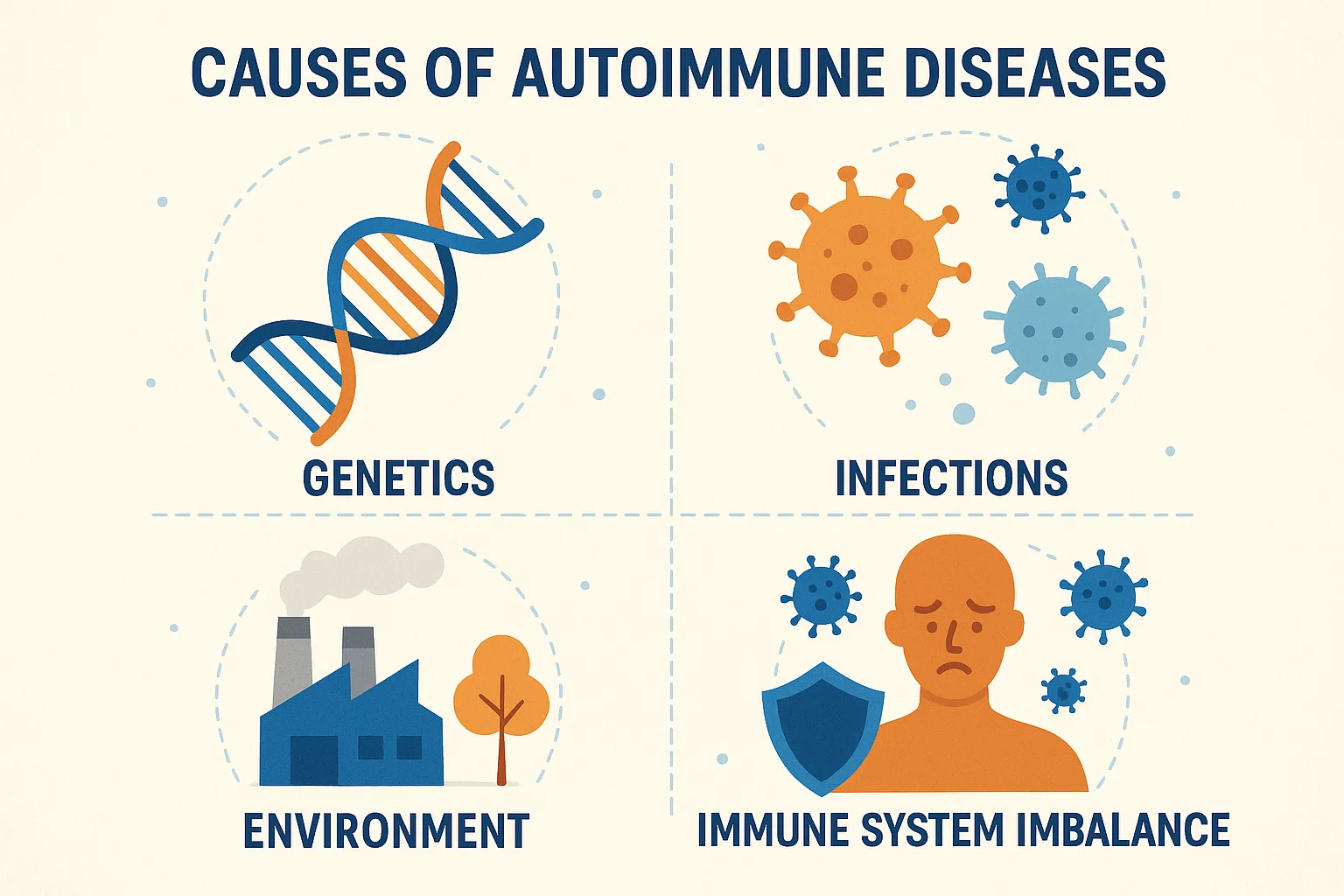
Genetic Factors
Your risk of developing an autoimmune disease may be in the family. Researchers identified certain genes that predispose some individuals to become ill. Yet possessing the genes is not a certainty—you need something else to set it off.
Environmental Influences
Something around you—such as a virus, certain toxins, or smoking—can trigger an autoimmune issue in somebody who’s predisposed to it. Certain infections or toxins can mislead your immune system to fight your body.
Hormonal Factors
Women are more likely to have autoimmune diseases than men, and that says a lot about hormones. Hormonal changes during puberty, pregnancy, or menopause can trigger or aggravate these diseases.
Gut Health and Microbiome
There is a world of bacteria inside your belly that regulate your immune system. From a 2019 Nature Reviews Immunology study, when this gets out of balance, it can actually compel your immune system to battle your own body. That makes what happens in your gut more important than we ever knew.
Symptoms and Diagnosis
Common Symptoms
Most autoimmune diseases share common symptoms. These include:
- Fatigue
- Pain or swelling, particularly in the joints
- Skin changes or rash
- Gastrointestinal disturbances
- Low-grade fever
- Swollen lymph glands
Because these symptoms are so nonspecific, it’s easy to overlook what’s really occurring.
Diagnostic Procedures
Certainly, physicians look back over your history and determine your symptoms. They’ll take a blood test to detect antibodies—stimuli that show your immune system is fighting back against you. They can even test for inflammation levels or examine single organs. X-rays or MRIs, or a biopsy (removing a small sample from your body surgically), may be needed.
Challenges in Diagnosis
Autoimmune disease is insidious. It strikes you and vanishes, and its signs can present similarly to so many other conditions. That makes it rather simple to misdiagnose. It’s not a bad thought to demand that something is amiss if you believe it, and if you have to, attempt a second opinion.
Treatment Alternatives
Medications
Treatment is usually a matter of calming your immune system and managing symptoms:
- Pain medications like ibuprofen
- Steroids to quickly reduce inflammation
- DMARDs (Disease-Modifying Antirheumatic Drugs) to slow the rate of the disease
- Biologics: newer medications produced from living cells that quiet certain parts of the immune system
The goal is to have you live better and avoid long-term harm.
Lifestyle Changes
Small changes in day-to-day life can make a huge difference:
- Eat whole, balanced foods
- Be active, with exercises your body can tolerate
- Sleep lots
- Deal with stress
In addition, quitting smoking and cutting back on alcohol may be helpful.
Alternative Therapies
Some people also find an added sense of comfort with acupuncture, massage, yoga, or meditation. They are not a replacement for medication, but they can improve overall health and minimize discomfort or tension.
Role of Patient Education
Educate yourself on your condition. The more you know about your disease and your treatment, the better you will be able to collaborate with your doctors. Educated patients are safer and fare better in the long term.
Living with Autoimmune Diseases
Taking Charge of Symptoms
Living with autoimmune disease is living with an attitude of awareness—to be aware of symptoms, follow your treatment plan, and be aware of what causes flare-ups. Regular visits to your doctor keep things in line.
Support Networks
Having supportive folks makes it all worth it. Supportive family and friends, or support networks on the web where you can share with others who understand what you’re experiencing, are all welcome.
Mental Health and Coping
It’s difficult on an emotional level to be ill all the time. It is okay to be tired, mad, or depressed. Going to a counselor, having things in your daily life that are good for your mind, and doing some things for yourself are absolutely vital.
Recent Research and Developments
Advances in Treatment
We have improved medications every year. Biologics, small molecule drugs, and other newer drugs improve at curing more specifically and with fewer side effectations than past medications.
Current Studies
Scientists are working at a sprint to learn more about how genes, gut microbes, and the environment set these diseases in motion. New clinical trials are attempting vaccines, gene therapies, and novel drugs—all with the goal of being able to allow those who suffer from autoimmune diseases to live more comfortably.
Preventive Measures
Diet and Nutrition
There is no single diet that heals autoimmune disease, but everybody knows to eat lots of fruits, vegetables, whole grains, lean protein, and healthy fat nourishes your immune system. Most individuals have anti-inflammatory diets which maintain foods low in sugar, processed foods, and refined carbohydrates.
Regular Exercise
Being active builds strength, decreases joint pain, lessens fatigue, and improves mood. Even simple exercises such as swimming, walking, or stretching can improve your health.
Stress Management Techniques
Stress can lead to flares, so healthy relaxation skills are required. Mindfulness, hobbies, breathing, deep stretching—anything that facilitates relaxation is a positive.
Future Outlook
New Trends in Autoimmune Research
The future looks promising. Scientists are experimenting with gene editing, personalized therapies specifically for each individual, and even mending tissue. Advances in the gut microbiome could unlock prevention as well.
Conclusion
Autoimmune illnesses are complicated, but there is hope. A large overview in Frontiers in Immunology (2024) found that contracting disease early, getting treatment from many specialists, and understanding your disease gives the best opportunity at being well. This shows why teamwork—between you, your doctors, and researchers—truly works. If you find yourself with unusual, inexplicable symptoms, don’t delay. Early physician visits can cause you to start searching sooner. With the right medical care, lifestyle modifications, and support system, most of those who suffer from autoimmune diseases are active, healthy living beings.