Fatty liver disease, also referred to as NAFLD, or non-alcoholic fatty liver disease, is a condition affecting a large part of the population and is becoming increasingly common. What starts off as deposition of fat in the liver may silently advance into serious conditions. Knowledge regarding fatty liver stage 2 and fatty liver stage 3 is very important in preventing severe damage.
It is important to know the signs of liver fibrosis and follow the development of a fatty liver to be able to intervene before it gets worse. The stages may appear harmless in the early going, but when fibrosis sets in, the chance of liver failure or worse, cancer, is increased. That’s why it is important to grasp what happens in the advanced stages of a fatty liver.
What is Fatty Liver Disease?
Fatty liver disease is a disorder wherein the accumulation of excess fat inside the liver cells impairs the normal organ function. The causes that could bring this about might be obesity, insulin resistance, type 2 diabetes, high levels of cholesterol, a sedentary lifestyle, and poor eating habits. Doctors classify it as fatty liver disease when more than 5%–10% of the liver cells contain fat. Chronic inflammation and scarring due to this condition could lead to advanced liver damage if not managed early.
There are two major kinds of fatty liver diseases: non-alcoholic fatty liver disease and alcoholic fatty liver disease. NAFLD is due to metabolic reasons and is independent of the high consumption of alcohol. It has become the most prevalent liver disease worldwide, and mainly among individuals affected by lifestyle diseases. AFLD, however, arises due to chronic alcohol intake that interferes with the metabolism and induces over-deposition of fat within the liver. Despite the fact that both conditions have different causes, they can follow a similar course of development and lead to the same kind of damage to the liver.
Diagnosis of fatty liver needs grading and staging to establish the extent of the disease. Grading describes the percent of fat in the liver, while staging describes the specific amount of scarring or damage to the liver. According to the US National Institutes of Health, staging helps in prognosis and management, especially in patients who are at risk of progressing into fibrosis or cirrhosis.
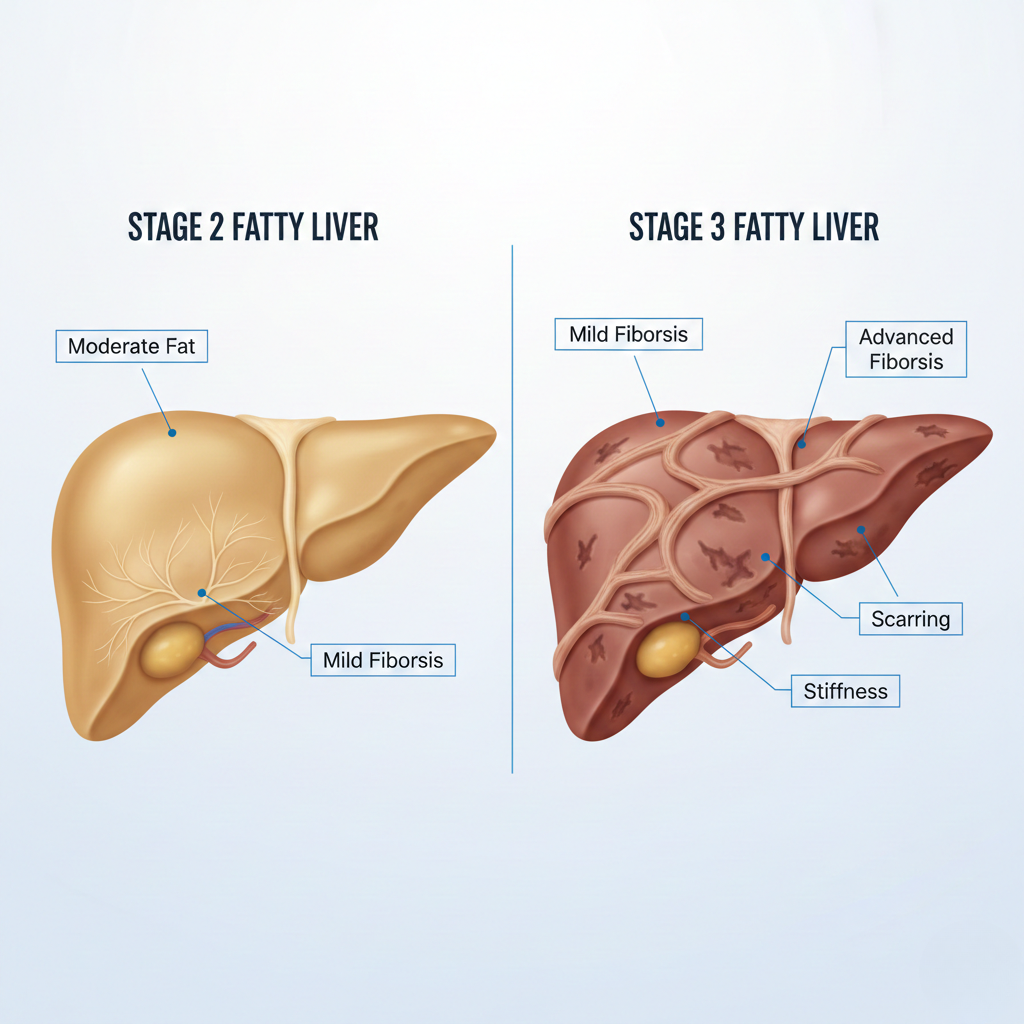
Understanding Stage 2 Fatty Liver
Stage 2 fatty liver is considered to be a moderate fibrosis condition wherein fat buildup inside the liver has progressed far enough to start causing structural changes and mild scarring. At this stage, physicians usually notice an increase in liver stiffness and fat deposition, often topping 20%-30% of liver tissue. Although the liver can still function, damage at this point has stopped being merely fatty accumulation; rather, true fibrosis, or the formation of scar tissue, has commenced, marking that the disease is indeed progressing from simple fatty liver to a more serious condition.
Symptoms at Stage 2 of fatty liver include nonspecific signs such as easy fatigability, mild right-sided abdominal discomfort, unexplained weakness, or gastrointestinal disturbances. Specialists outline that the majority of patients are asymptomatic, and this means that the condition can get worse without regular check-ups being performed.
The importance of early diagnosis of stage 2 fatty liver is that it is still reversible, provided timely intervention is done. It includes a healthy diet, reduction of body fat, regular exercise, treatment of metabolic disorders, and abstinence from alcohol. These can considerably delay or even reverse the process of fibrosis. Medical guidelines underline that intervention at this stage can prevent further degeneration into stage 3 or cirrhosis, where the chances of damage reversal are minimal.
Unpacking Stage 3 Fatty Liver
Stage 3 is advanced fibrosis in which scarring has spread extensively enough to cause significant distortion in the liver structure, although it has not reached complete cirrhosis. Medical imaging, for example, FibroScan, MRI elastography, or ultrasound-based elastography, will distinctly show increased liver stiffness and an irregular texture with visible scarring patterns. In comparison with stage 2, more pronounced changes are seen in this stage, with the liver starting to lose its capacity for regeneration.
At this stage, symptoms are more identifiable and can include chronic fatigue, abdominal pain on the right side, swelling of the legs or abdomen, unexplained weight loss, nausea, gastrointestinal problems, and a loss of appetite. Blood tests can also show high liver enzymes, a low platelet count, or other signs that there has been a decrease in liver function. Overall, these warning signs tend to indicate a more serious inflammation and an increase in scar tissue that impairs normal metabolic functions of the liver. Some patients develop jaundice, along with darkened urine or itchy skin, as toxins are harder for the body to filter from the system.
The risks in stage 3 are much higher compared to the earlier stages. If left untreated, fibrosis may turn into stage 4-cirrhosis, where one’s liver has suffered irreversible damage. Complications can be anything from portal hypertension and internal bleeding to liver failure and increased risk of liver cancer. Early medical intervention with scheduled monitoring and lifestyle adjustments remain critical for hindering or halting further deterioration.
Direct Comparison: Stage 2 vs. Stage 3
Below is a clear comparison between Stage 2 and Stage 3 of fatty liver disease, with the changes taking place in the body as the disease progresses.
| Feature | Stage 2 Fatty Liver | Stage 3 Fatty Liver |
|---|---|---|
| Fat Infiltration | Significant fat buildup (often 20–30% or more), with early fibrosis beginning | Extensive fat accumulation with advanced fibrosis spreading across liver tissue |
| Liver Structure Changes | Mild scarring, liver still structurally functional | Noticeable distortion of liver architecture, stiffening visible on scans |
| Symptoms | Often mild — fatigue, slight abdominal discomfort, elevated enzymes | More evident — persistent pain, swelling, metabolic issues, jaundice in some cases |
| Reversibility | Highly reversible with timely intervention | Reversible only in some cases; harder to reverse due to advanced scarring |
| Major Risks | Progression to advanced fibrosis if untreated | High risk of cirrhosis, liver failure, and liver cancer |
Diagnostic Techniques
Diagnosis at Stage 2 may include :
- Ultrasound of the liver
- FibroScan measuring moderate stiffness
- MRI-PDFF to quantify fat percentage
- Blood tests showing mildly raised liver enzymes
Diagnosis in Stage 3 may include:
- MRI elastography demonstrating advanced tissue stiffening.
- FibroScan with high stiffness scores
- Ultrasound demonstrating structural distortion
- Blood tests, which can reveal metabolic and functional imbalances
Preventing the Progression From Stage 2 to Stage 3
- Low sugar, low fat, balanced diet
- Lose 7–10% of body weight if not the correct weight for your body
- Improve insulin resistance through diet and exercise.
- Avoid alcohol completely.
- Monitor liver enzymes every 3–6 months
- Manage chronic conditions, like diabetes, high cholesterol, and obesity, upfront.
Early lifestyle and medical intervention serve as a person’s strongest defenses against advancing into irreversible liver damage.
The Latest on Fatty Liver Research
New Diagnostic Tools: Biomarkers and Imaging
Recent advances have targeted non-invasive testing with a goal to minimise the need for biopsy. Quantitative imaging of the liver, including MRI-PDFF and magnetic resonance elastography, provided more precise estimates of liver fat and stiffness, respectively. Point-of-care elastography – FibroScan – is widely used for monitoring fibrosis longitudinally. The blood-based biomarkers of fibrosis, such as enhanced liver fibrosis score and FIB-4 index, were iteratively improved and combined with imaging for early detection of clinically significant fibrosis.
Emerging treatments and drugs on the horizon
Over the past years, pharmacology has transitioned from aspirational candidates to clear approvals and late-stage testing. Selected agents-thyroid hormone receptor agonists, FXR agonists, GLP-1 and dual GIP/GLP-1 agonists, and FGF21 analogues-are promising classes that reduce liver fat and/or improve fibrosis in clinical testing. Compounds including resmetirom and several drugs of the GLP-1 class are currently under regulatory review or have delivered positive phase-2/3 testing. For the first time, this may position drug therapy to augment lifestyle measures in patients with progressive disease.
Importance of personalized medicine
Fatty liver is heterogeneous, and genetics, metabolic profile, and comorbidities shape risk and treatment response. Precision approaches using genomics, metabolic phenotyping, and longitudinal non-invasive testing pave the way for personalized choice of therapy, such as prioritizing weight-loss agents over antifibrotic drugs, and enhance risk stratification. US government-funded research programs, like those from NIDDK/NIH, are actively funding studies to map the genetic drivers and biomarkers accelerating precision care. Personalized medicine is at the very core of translation from recent diagnostic and drug advances into improved outcomes in patients.
Impact on Emotional and Mental Health
A diagnosis of chronic liver disease is emotionally stressful, especially when it is already at an advanced stage. Indeed, many patients suffer from feelings of fear and insecurity about the future, but also from guilty feelings due to lifestyle or irritability in those whose symptoms interfere with everyday activities. The thought of having a “silent” disease that might continue to progress without warning can further heighten stress. All these reactions are understandable, but if not dealt with properly, they will negatively affect health status in general and complicate adherence to treatment and lifestyle modification.
Coping with anxiety and stress requires intentionality. Healthier daily routines, keeping open communication with healthcare providers, meditation or deep breathing, and journaling of feelings give one a sense of control. Realistic habits, such as gradual improvements in diet, more physical activity, and tracking progress, actually empower the patient without feeling overwhelmed in the process. You need to remind yourself that behaviors take time to change and that improvements don’t have to be huge to be constructive.
Support systems are as important as medical care. Professional counselors, clinical psychologists, and mental health support teams that operate within a hospital setting and specialize in adjustment to chronic illness will benefit the patients. In-person and online liver disease support groups can help connect people who understand what it’s like and may help diminish feelings of isolation and provide encouragement. And with structured guidance, requisite emotional support, and follow-up, management of the fatty liver becomes a stronger mental journey rather than just a medical one.
Practical Steps to Manage Fatty Liver
- Your diet should be well-rounded, filled with vegetables, fruits, whole grains, lean proteins, nuts, and healthy fats.
- Decrease intake of refined sugars, processed foods, excess saturated fat, and alcohol.
- Aim for a 7-10% body weight reduction to realize an improvement in liver fat and a reversal of early fibrosis.
- Exercise 30–45 minutes at least 5 days a week; walking, cycling, swimming, going to the gym, or strength training.
- Regular exercise can, therefore, enhance metabolism, increasing the sensitivity of tissues to insulin.
Medical management
- Schedule follow-up blood tests and liver imaging studies: Ultrasound, FibroScan, and MRI Elastography.
- Take medications, if necessary, for diabetes, cholesterol, insulin resistance, or inflammation.
- Consult a hepatologist or gastroenterologist in moderate and advanced stages.
- Refer to a dietitian or liver specialist for individualized plans.
Screening and Self-care
- Monitor liver enzyme levels every 3–6 months.
- Practice good stress management: meditation, journaling, and therapy are just a few ideas.
- Improve the quality of sleep and return to normal daily activities.
- Stay updated and keep informing yourself about fatty liver to stay a step ahead.
- Instead, focus on long-term habits rather than quick fixes in the short run to avoid regression.
FAQs
What symptoms is the patient likely to experience?
- Oftentimes, there are no symptoms manifested in the early stages. Symptoms may include chronic fatigue, abdominal discomfort, digestive disturbances, or abnormal liver function tests.
How is a fatty liver tested?
- Tests often consist of liver blood panels, ultrasound, FibroScan, and MRI-based imaging. Physicians can combine tests in determining fat accumulation and fibrosis.
Can stage 2 or stage 3 fatty liver improve?
- Stage 2 is usually reversible with lifestyle modification and medical monitoring. The improvement of stage 3 is more difficult; it is, however, possible with aggressive treatment and monitoring.
What is the long-term prognosis?
- Early detection greatly improves outcomes. If left untreated, the disease can progress to cirrhosis or liver failure over time.
When should I go straight to A&E?
- Seek immediate emergency care if severe abdominal swelling, jaundice, dark-colored urine, confusion, vomiting blood, or sudden weakness is present.
How often should routine follow-up be done?
- Most patients benefit from a medical review every 3–6 months with enzyme tests and imaging when necessary.
Interactive Resources and Tools
- Downloadable symptom checklists can be used by patients to monitor changes on a weekly or monthly basis.
- Routine monitoring logs help document diet, exercise, sleep, weight, and lab reports.
- Calculators for BMI, liver fibrosis risk, and metabolic score can facilitate the personalization of a care plan and allow measurements of progress.
- Many hospitals and health websites offer free printable resources for patient self-management.
Conclusion
Early recognition of the changes occurring in stage 2 and stage 3 fatty liver is critical for preventing long-term liver damage. Awareness of subtle symptoms, routine checkups, improvement in lifestyle, and timely medical support can bring down or even reverse the development in many cases. Understanding their condition better enables patients to seek early care, take responsibility for their health, and develop habits that will help them preserve liver function for years to come.